Core Eye Services
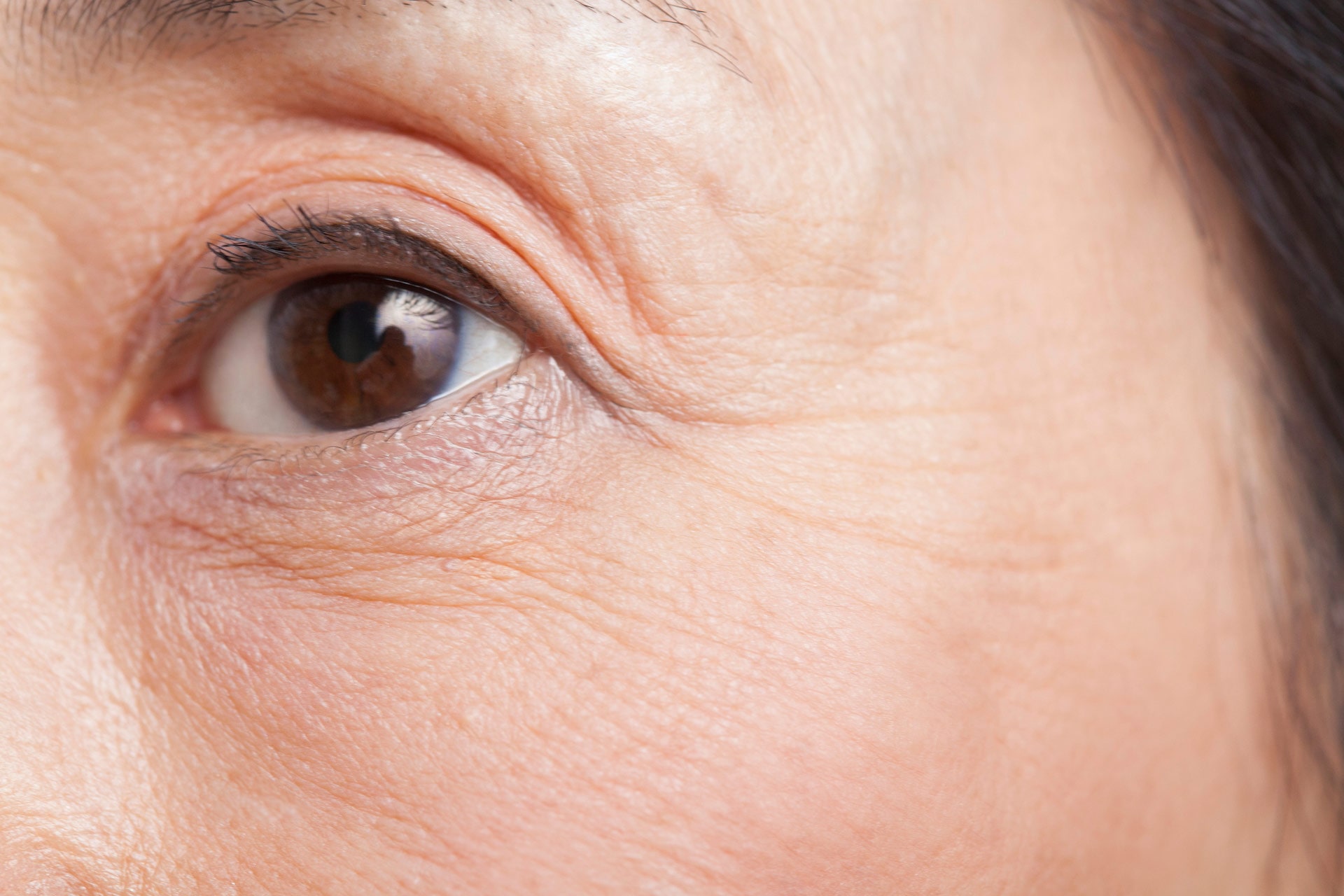
Cornea / External Disease
The conjunctiva is the clear tissue that covers the front surface of the eye (the white part) and the inner surface of the eyelids, while the cornea is the transparent part of the eye that covers the front portion and pupil. The cornea is what focuses most of the light that enters the eye.
The Primary Functions of the Conjunctiva are:
- Keeping the front surface of the eye lubricated
- Keeping the inner surface of the eyelids lubricated so they open and close easily
- Protecting the eye from dust, debris, and infection
Top Three Cornea Problems
While there are several diseases that can affect the cornea (or part of it), the three most common issues that we see at Clarity Eye are:
- Infection
- Keratoconus
- Pterygium

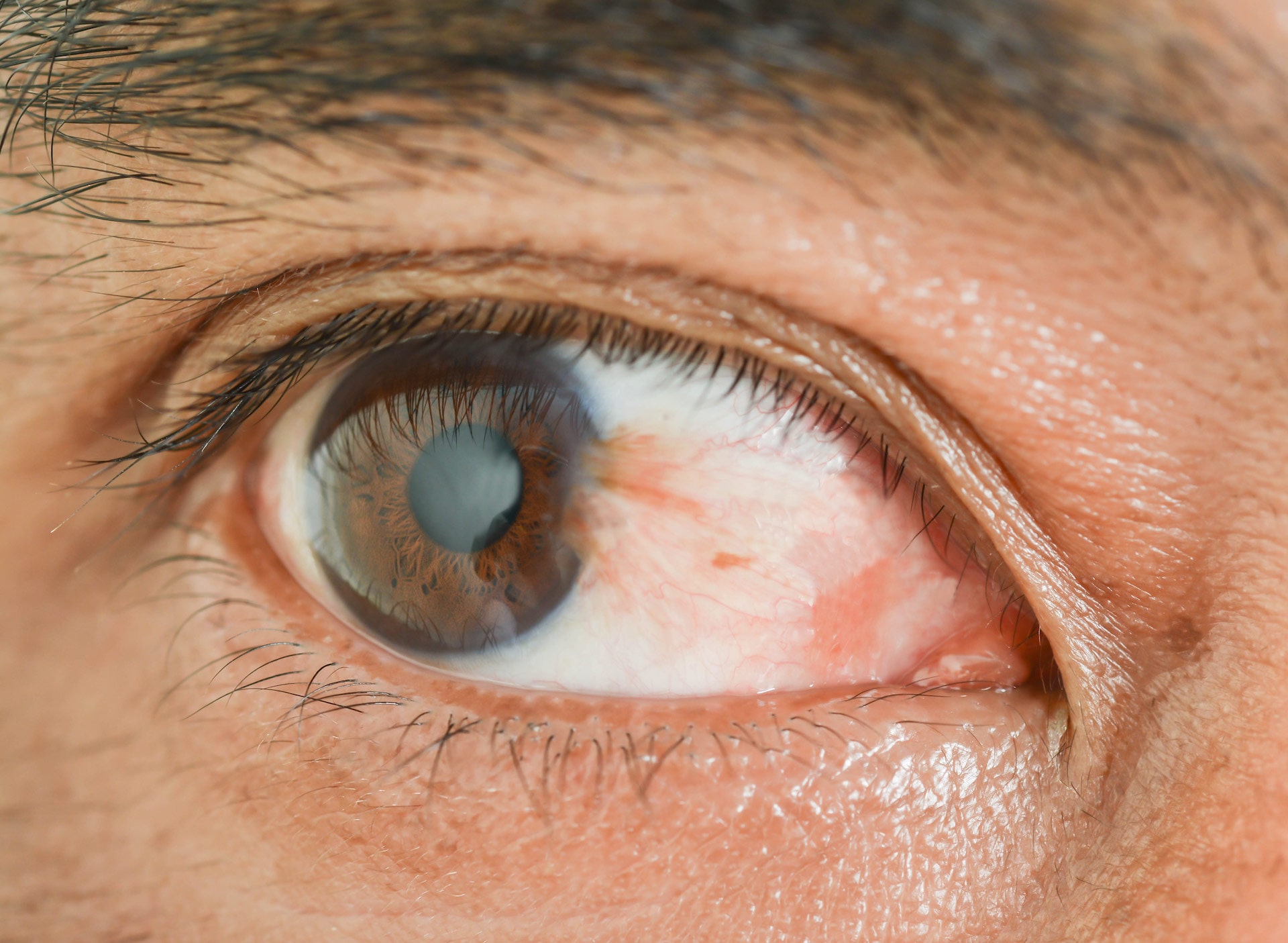
Infection
A healthy cornea can normally resist infection; however, if the cornea becomes injured through a poke in the eye or through a contaminated contact lens, a corneal infection, or keratitis, can occur. This can cause inflammation in the cornea and potentially lead to corneal scarring. In the most serious cases, keratitis can cause loss of vision or blindness, so it’s important to seek medical attention if you experience any signs of infection.
Causes of Corneal Infection:
Contact lens wearers are more prone to infectious keratitis by:
- Wearing contacts overnight
- Reusing contact solution
- Storing lenses in tap water that may be contaminated
Non-infectious keratitis can be caused by:
- Allergic reaction to deposits on the lenses
- Chemicals, including those in contact lens solution
- Dryness of the eyes
Symptoms of Corneal Infection:
- Blurry or hazy vision
- Itching and discharge
- Sensitivity to light
- Redness or bloodshot eye
- Very painful and watery eye
- White spot on the cornea
Keratoconus
Keratoconus is a slow, progressive thinning of the cornea in which the normally round, dome-shaped cornea thins and bulges outward, gradually forming a rounded cone-like shape. This change in shape bends the light as it enters the eye, impacting the cornea’s refractive capabilities. As a result, keratoconus can cause astigmatism or distortion, and nearsightedness or blurriness.
Blurred vision caused by keratoconus is different from blurred vision that is caused by other common refractive errors such as myopia or hyperopia. In its later stages, correcting vision, even with glasses or contacts, can be difficult, so early treatment is key.
Causes of Keratoconus:
While researchers have come up with a few theories, the exact cause of keratoconus is not really known. It’s believed that genetics and the environment both play a role in this disease.
Symptoms of Keratoconus:
Keratoconus can occur in one or both eyes, often beginning in a person's teens or early twenties (but can start any time). Early signs to look out for:
- Blurry vision
- Blurred vision not corrected with glasses
- Frequent change in eye prescription
- Increased light sensitivity
- Difficulty with night driving
- Halos and glare especially at night
- Eye strain
- Headaches and general eye pain
- Eye irritation
In the advanced stages of keratoconus, sudden clouding of vision in one eye lasting weeks or months might be experienced. This is called acute hydrops. Superficial scars can also form at the apex of the corneal bulge resulting in more vision impairment. Like all eye conditions, the earlier a diagnosis can be made, the better the outcome for the patient.
Pterygium
A pterygium is a non-cancerous growth of pink, fleshy tissue on the conjunctiva— the clear tissue that lines your eyelids and covers your eyeball. Commonly referred to as surfer’s eye, this condition can affect anyone who spends a lot of time outdoors and can occur in one or both eyes. Growth may be slow throughout a person’s life, while others stop growing after a certain point.
Causes of Pterygium:
While the exact cause is unclear, prolonged exposure to ultraviolet light plays a key role. Irritants like dust and wind and dry eyes also play a factor.
Symptoms of Pterygium:
Sometimes it just appears without any symptoms, and others may experience the following sensations:
- Burning
- Grittiness
- Itchiness
- Redness
- Feeling that something’s in the eye
If the growth extends to the pupil, it may cause blurry vision or double vision.
Treatments of Cornea Conditions
The two most common cornea treatments performed at Clarity Eye are:
- Pterygium
- Transplants
Pterygium
Once a pterygium diagnosis is made, treatment may not be necessary depending on severity. For cases with redness or irritation, over the counter eyedrops/ointments or prescription steroid medication may be required.
For a patient who’s experiencing discomfort or vision problems or wants it removed for cosmetic reasons, one of our highly qualified surgeons at Clarity Eye can remove it through an outpatient procedure. This minimally invasive surgery generally takes no more than 30 minutes.
What to Expect During Ptergium Surgery
- You will be given mild oral sedation and your eyes numbed.
- The surrounding eye area will be cleaned.
- The pterygium along with some associated conjunctival tissue will be removed.
- A graft will be used from an area with healthy conjunctiva underneath the patient’s eyelid to fill the area where the pterygium was removed.
- The graft will be secured in its place with the use of either sutures or fibrin glue, reducing the possibility of a recurring pterygium.
Recovery
Depending on technique used in surgery, recovery is normally a couple of weeks to a couple of months for complete healing, but you can return to work or normal activities within a few days. You’ll be provided with aftercare instructions and a follow-up appointment schedule post-surgery.
Corneal Transplants
A cornea transplant, known as a keratoplasty, removes the diseased, infected, or scarred part of the cornea and replaces it with corneal tissue from a donor, or in some cases, with an artificial cornea (keratoprosthesis). The transplant procedure restores vision, along with relieving pain and other symptoms associated with cornea diseases. While the success rate is high for corneal transplants, there’s a small risk of complications, including a rejection of a donor cornea, requiring additional medical treatment or another cornea transplant.
A number of conditions can be treated with a cornea transplant, including:
- Outward corneal bulges (keratoconus)
- Cornea scarring caused by infection or injury
- Cornea swelling
- Corneal ulcers unresponsive to medical treatment
- Thinning or tearing of the cornea
- Certain medical/hereditary conditions
There are different methods used to perform a cornea transplant. Your surgeon at Clarity Eye will discuss what’s right for you based on your personal situation. Surgery usually takes less than an hour with patients able to leave same day; however, in some circumstances, an overnight stay may be required.
What to Expect During a Cornea Transplant
You'll either be given a sedative to help you relax and a local anesthetic to numb your eye, or you'll be put to sleep. Regardless of method, you shouldn't feel pain. Once your cornea transplant is completed, you can expect to:
- Receive medications – eyedrops and, sometimes, oral medications – to help control infection, swelling and pain post-surgery and help prevent cornea rejections
- Wear eye protection to protect eye during healing process
- Lie on your back to help ensure new tissue stays in place, depending on type of transplant
- Avoid injury – no rubbing or pressing on the eye
- See your doctor for follow-up appointments.
Signs to Watch Out for Post-surgery
Contact your surgeon immediately if you experience any vision issues or display signs of infection (fever, eye drainage or pain). Signs of cornea rejection to look out for include:
- Eye pain
- Redness in eye
- Cloudy vision
- Light sensitivity
Recovery
Most people can resume normal activities and return to work in about 1 to 2 weeks post-surgery; however, vision will still be blurry. Your doctor will provide you with a list of activities that you’ll need to avoid for a longer period. It may take three months or longer to see clearly and realize the full benefits of surgery.
